Psoriasis is more than just a skin condition—it’s a chronic autoimmune disease that affects over 8 million Americans. For many, it’s not only the visible red patches or flakes that cause distress, but also the emotional toll of living with a condition that can flare up anytime. If you’ve ever felt frustrated because your skin seems to “turn against you,” you’re not alone.
In this article, we’ll explore what psoriasis really is, what causes it, common triggers, treatment options, and how diet and lifestyle choices can help you manage symptoms more effectively.

What Is Psoriasis?
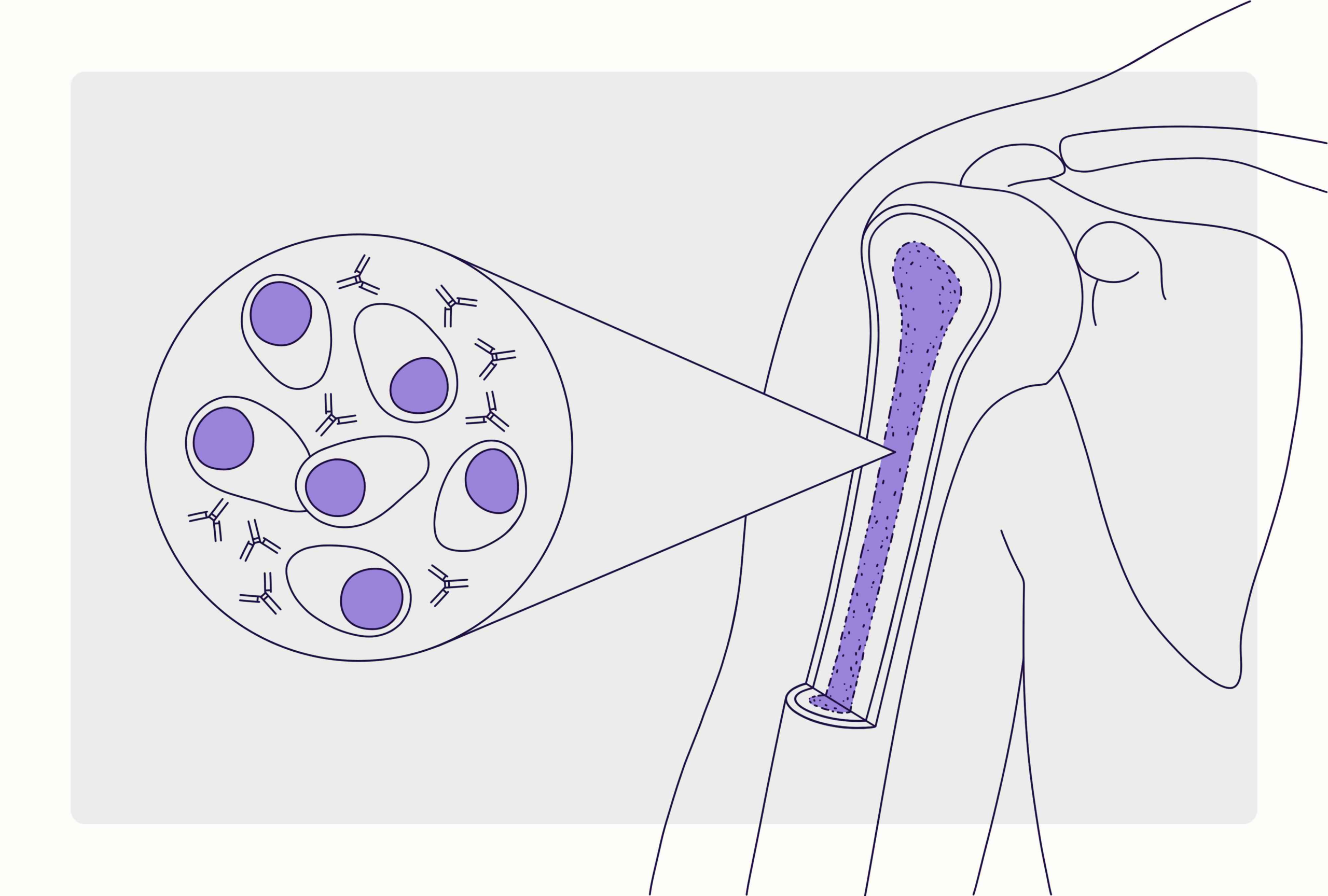
Psoriasis is a long-term inflammatory skin disease in which the immune system becomes overactive, speeding up the life cycle of skin cells. Normally, skin cells grow and shed every 28–30 days. In people with psoriasis, new cells form in just 3–4 days, causing them to build up on the surface and create thick, scaly, inflamed patches known as plaques.
These plaques often appear on the elbows, knees, scalp, lower back, and nails, but can occur anywhere on the body. Psoriasis is not contagious, but it can be uncomfortable, painful, and emotionally challenging.
Common Symptoms
Psoriasis symptoms vary from person to person, but common signs include:
- Red, raised patches of skin covered with silvery-white scales
- Itching, burning, or soreness around affected areas
- Cracked, dry skin that may bleed
- Thickened or ridged nails
- Joint pain or stiffness (a sign of psoriatic arthritis)
Some people experience mild symptoms limited to small areas, while others have widespread inflammation that significantly affects their quality of life.
What Causes Psoriasis?
Psoriasis is an autoimmune condition, meaning the immune system mistakenly attacks healthy skin cells. The exact cause is unknown, but several factors play a role:
- Genetics: If one or both parents have psoriasis, your risk increases.
- Immune system dysfunction: Overactive immune cells cause inflammation and excessive skin cell growth.
- Environmental triggers: Stress, infections, skin injuries, or certain medications can trigger flare-ups.
- Lifestyle factors: Smoking, alcohol, and obesity can worsen symptoms.
Types of Psoriasis
There are several forms of psoriasis, each with distinct features:
- Plaque Psoriasis (Psoriasis Vulgaris): The most common type, causing raised, scaly patches.
- Guttate Psoriasis: Small, dot-like lesions that often appear after a throat infection.
- Inverse Psoriasis: Smooth, shiny patches that form in skin folds (like underarms or groin).
- Pustular Psoriasis: White pustules filled with pus, often on hands and feet.
- Erythrodermic Psoriasis: A severe, widespread type that can be life-threatening and needs urgent medical care.
Common Triggers for Psoriasis Flare-Ups
Psoriasis tends to come and go in cycles, with periods of remission followed by flare-ups. Common triggers include:
- Stress and anxiety
- Cold, dry weather
- Skin injuries or infections
- Certain medications (like beta-blockers or lithium)
- Alcohol consumption
- Smoking
Identifying and avoiding your personal triggers is a key part of managing the disease.
Treatment Options
Although there’s no permanent cure for psoriasis, effective treatments can help control symptoms and prevent flare-ups.
- Topical Treatments:
- Corticosteroid creams reduce inflammation and itching.
- Vitamin D analogs (like calcipotriene) slow cell growth.
- Moisturizers prevent dryness and cracking.
- Light Therapy (Phototherapy):
- Controlled exposure to natural or artificial UV light can slow down skin cell production.
- Systemic Medications:
- For moderate to severe psoriasis, oral or injectable medications like methotrexate, cyclosporine, or biologics (adalimumab, etanercept, ustekinumab) target immune system overactivity.
- Biologic Therapies:
- Newer treatments that specifically block inflammatory pathways, showing excellent results in reducing symptoms.
Your dermatologist will recommend a personalized plan depending on the type and severity of your psoriasis.
Diet and Lifestyle Tips for Managing Psoriasis
While no diet can cure psoriasis, nutrition plays an important role in reducing inflammation and maintaining overall health.
Foods That May Help:
- Fatty fish (salmon, mackerel, sardines): Rich in omega-3 fatty acids that fight inflammation.
- Fruits and vegetables: Especially berries, spinach, and kale, which are high in antioxidants.
- Whole grains and legumes: Provide steady energy and support gut health.
- Olive oil and nuts: Healthy fats that can help soothe inflammation.
- Turmeric: Contains curcumin, a natural anti-inflammatory compound.
Foods to Avoid:
- Processed and fried foods
- Sugary snacks and drinks
- Red meats and dairy (for some people)
- Alcohol and smoking
Other Helpful Habits:
- Keep your skin moisturized, especially in dry weather.
- Take lukewarm baths with oatmeal or Epsom salt.
- Manage stress through meditation, yoga, or light exercise.
- Get adequate sleep to support your immune system.
When to See a Doctor
If you notice persistent red or scaly patches that don’t improve with over-the-counter creams, or if your joints start to ache or swell, it’s important to consult a dermatologist or rheumatologist. Early treatment can help prevent complications like psoriatic arthritis, which can cause permanent joint damage.

Conclusion: You Can Take Back Control of Your Skin
Living with psoriasis can be frustrating, but it doesn’t have to define you. With the right treatment, a healthy lifestyle, and emotional support, you can significantly reduce flare-ups and feel confident in your skin again.
Remember—psoriasis is not your fault, and you’re not alone. The key is learning how to manage your body’s signals and making small, consistent choices that lead to big improvements in your health and well-being.